2 Predictions & 4 Trends: The Future of Telehealth Has Arrived
Are you sick of hearing about the unprecedented growth of Telehealth? Punny, I know! Like working from home – the technology has been available, but most didn’t transition to it because they didn’t have to.
With the advent of a pandemic, Telehealth has experienced a rapid uptick in utilization, funding and popularity (it’s all the rage, dahling).
While I’m not an “expert,” I’ve owned a company that provides Telehealth for 10+ years, we have coordinated over 150,000 telehealth visits, and saved our clients $80+ million in unnecessary claims.
With that, I’ll share 4 trends and 2 predictions…
PREDICTION #1
Telehealth will be used for all manner of healthcare and medical needs. Way back in 2019 at the HLTH Conference, Dr. Peter Fleischut, SVP & Chief Transformation Officer, New York - Presbyterian Hospital had this to say…
“The time will come when we don’t talk about ‘in-person health’ and ‘Telehealth’ - when we just call it ‘health.’
The question isn’t “WILL it happen?” the question is “WHEN will it happen?” Is it 2021 or 2031? We don’t know, but…
TREND #1: HEALTHCARE COST & ACCESS TRENDS
No healthcare article would be complete without some info on healthcare cost trends! If you’re an employee benefits consultant, you already know all this stuff, so feel free to skip to trend #2!
Healthcare spend has been climbing pretty consistently since 2000 and there’s no real end in sight.
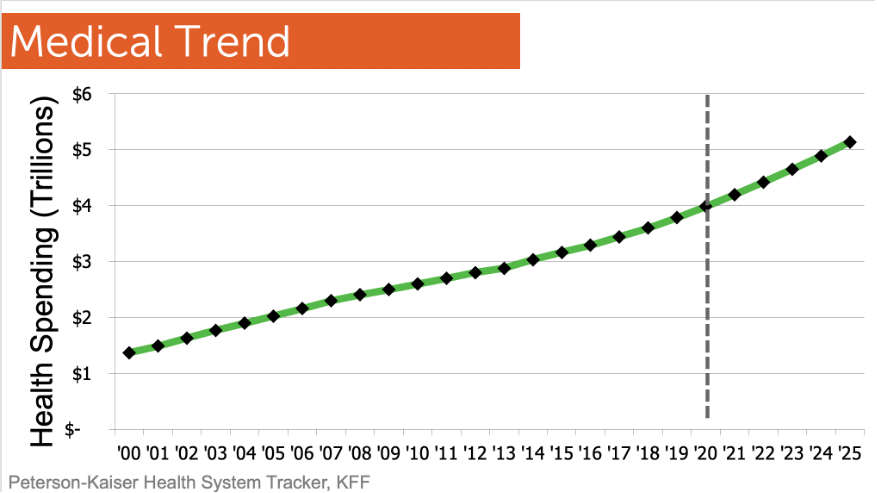
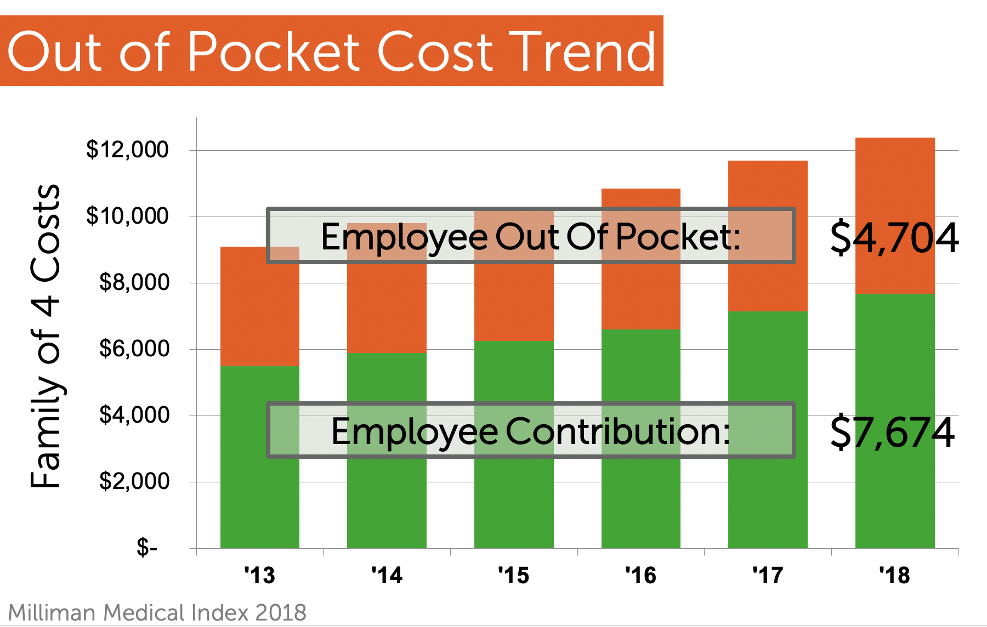
This is a struggle for employers and their employees. In the last 5 years, employees have seen a 40% increase in overall costs – not just in their out-of-pocket costs, but also their contributions to the insurance premium. This is a curve that needs to be flattened, but there’s really no end in sight. Even before COVID-19, people were being driven to change their habits.
And we’ll pile on top of that: when employees go to access the system, they are having a harder time finding care…
- The Association of American Medical Colleges estimates that America will be short 40,800 to 104,900 doctors by 2030.
- The wait time to see a doctor has increased from 18 days in 2014 to 24 days in 2017 (Merritt Hawkins Survey) – that’s a 30% increase. More recent stats aren’t available, so you can imagine what it is a couple years later.
- Before COVID-19, there were 1 BILLION Google searches daily for health information.
Bottom line: Americans are paying a lot more money for less access to care and care that’s harder to get.
TREND #2: INCREASED NEED FOR TELEHEALTH
So here comes Telehealth: an efficient, simple and inexpensive way to access care. For 10 years, we’ve said that 70% of doctor visits could be handled by phone or video. Now we’re starting to see it in action. The problem has been usage.
According to Mercer, employers reported an average utilization rate of 9% in 2019 and 7% in 2018. We’ve all heard the news about the March/April 2020 spike in usage. Most report that usage receded after the initial uptick. This could be because people aren’t experiencing normal sickness due to social distancing, mask wearing and incessant hand washing.
Most studies show that Americans and doctors have been happy with their telehealth experience, so only time will tell what future usage trends look like. The access to care stats shared abovein trend #1, alongside a new comfort level with Telehealth and access to the technology, indicate that usage will continue to increase.
Sooner or later, the threat from COVID-19 will go away. But the need to rethink where and how we deliver healthcare won't.
TREND #3: HOW PEOPLE WILL USE TELEHEALTH
You probably already know the basics of Telehealth for urgent care medical issues. Most employee benefits brokers have introduced Telehealth to their groups over the past few years. Many have sold it as part of a health plan with a visit fee (until recent fee changes during the pandemic). The top diagnoses are nasal congestion, flu, cough, UTI, allergies, pink eye, sinus issues, bronchitis, upper respiratory infection and ear infection.
Now that the idea has been successful, Telehealth is being expanded to many other areas of support. Below are some up and coming types of Telehealth…
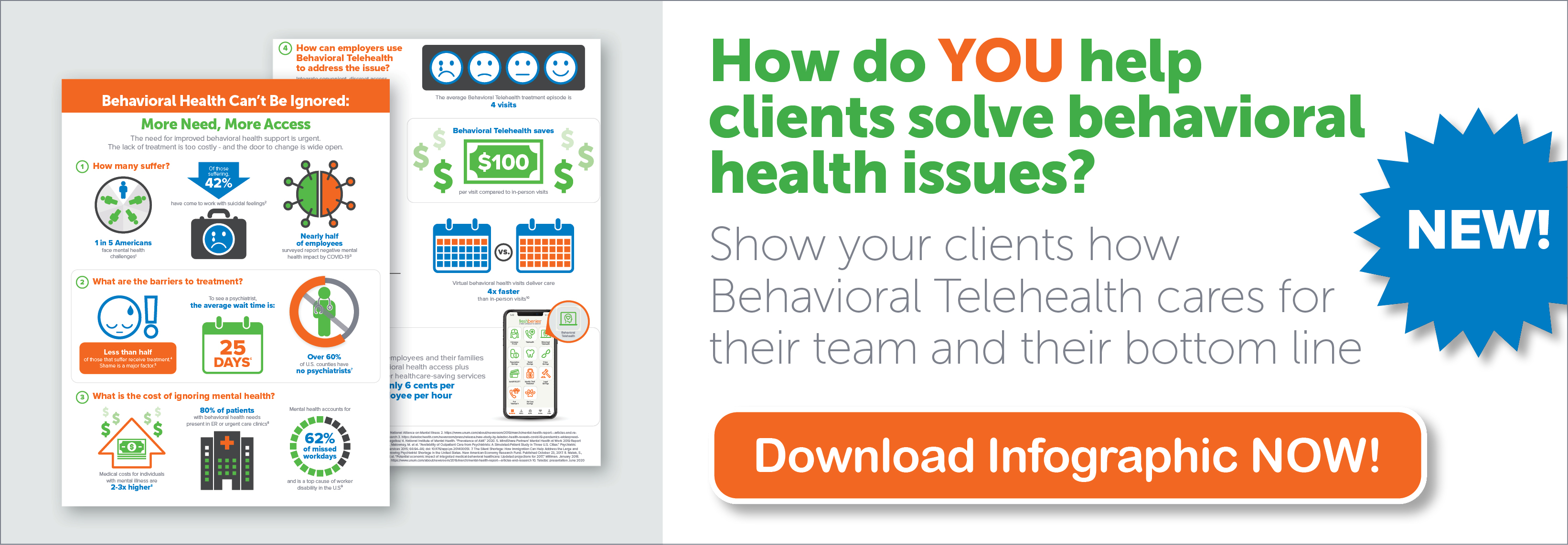
- Behavioral Telehealth: video call with a counselor, psychologist or psychiatrist at a fraction of the cost of in-person. Learn more here.
- Dermatology: acne, rashes, suspicious spots and moles, eczema, rosacea, psoriasis, alopecia, etc.
- Pediatrics: parents can use Telehealth for kids the same way they use it for themselves.
- Physical therapy: there are many physical therapy “deserts” in our country. Licensed physical therapists help work with patients remotely to improve muscle or joint conditions – back, wrists, knees, hips, neck, shoulders, arthritis, etc.
- Second opinions: expert medical opinions from doctors for patients who are unsure about a diagnosis, need help deciding on a treatment option, want advice or a second opinion, or for patients who’ve been admitted into the hospital and need expert guidance
- Teledentistry: antibiotics for abscesses, advice about dental issues, navigating patients to dentists who are in-network and open for business.
- Vision: currently, vision providers can answer questions and diagnose eye infections. In the future, could an exam be done? Ophthalmologists aren’t bullish, but if pandemics continue and as technology improves, I bet they’ll figure it out.
- Primary care: nearly 27% of U.S. adults and as high as 45% of adults under 39 don’t have a primary care physician. This type of Telehealth allows patients to develop ongoing relationships with virtual primary care doctor who can do annual wellness screenings, manage chronic care conditions, order labs, refer to specialists and provide follow-up care. Remote exam kits that include an exam camera, forehead infrared thermometer and otoscope, stethoscope and tongue depressor allow patients to transmit test results to an electronic health record for the doctor to see and/or monitor.
- Sexual health: help with everything from sexually transmitted diseases to erectile dysfunction.
- Fertility: from birth control and pre-conception counseling, to fertility, pregnancy, lactation, and returning to work after baby. And if all that doesn’t work out, there’s help with adoption services.
- A few others…
- Meds management and prescription renewal
- Chronic condition management
- Smoking cessation
- Wellness and weight management
- Hair loss counseling
- Home healthcare
- Post-hospital discharge
- Post-surgical follow-up
And don’t forget your furry family! Pet Telehealth can help with behavioral issues (for example, how to introduce a new pet to current pets or how to stop bad behavior), or determine which situations require after-hours attention or can wait until Monday.
Finally, while not specifically “Telehealth,” Advocacy programs give expert, personalized help to navigate healthcare via phone or email. An Advocate can find quality, local, in-network providers, research accurate procedure pricing, find prescription savings options, negotiate medical bills, and more. Check out this infographic for more.
TREND #4: HOW PEOPLE WILL ACCESS TELEHEALTH
Americans are accessing Telehealth in multiple ways these days. Here are a few examples…
- Telehealth companies: you know the usual suspects (Doctor On Demand, MDLive, Teladoc, American Well) and new ones are popping up left and right. Also, visit prices are increasing, and many are introducing the new services I just covered.
- Health plans: some use a telehealth company to fulfill the service, others have it built in (i.e. Kaiser).
- Standalone plans (like freshbenies): these typically have a stronger member engagement program and higher utilization, provide $0 visit fees, eliminate the need to create a new account as health plans change, and provide utilization stats (health plans don’t typically share for groups under 100)
- Doctor scheduling services (like Zocdoc and Doctor.com): in the past, these services have helped people find local doctors. Now they’re offering Telehealth appointment scheduling with those participating doctors. They’re navigating people to doctors – and doctors pay these services for access to the technology and the lead.
- Direct Primary Care: these primary care practices typically charge patients a flat monthly or annual fee in exchange for access to a broad range of primary care services – most times that includes Telehealth.
- Current PCPs or Specialists: many Americans are now using Telehealth with their own doctors. Practices are using this time to test Telehealth since federal regulators have relaxed HIPAA rules. But implementing this on a large scale isn’t easy – it takes appropriate technology, a trained staff and patients, and the introduction of new workflows. As a result, doctors may be hesitant to make the investment if there is uncertainty around Telehealth visits being covered by health plans and government programs. There’s more flexibility for reimbursement now, but those changes are temporary. If doctors knew their future Telehealth reimbursement wouldn’t be on par with an in-person visit, they might decide against those investments and accelerate their switch back to in-person care.
- Hospitals: Telehealth is great for post-surgical and follow-up visits. Rural hospitals use Telehealth for specialties they don’t have in-house. Some hospital chains have sophisticated virtual monitoring so they can help patients faster without having as many healthcare workers on-site.
- Home health companies: remote monitoring for homebound patients or as a supplement to visiting nurse care.
That’s quite a list – and I’m sure I haven’t even run across MANY other options! Now, we have to figure out: who will pay for it?
TREND #5: WHO WILL PAY FOR TELEHEALTH
This topic is in hot debate as there are a lot of players and money at stake.
First, a side note on HSA regulations as they relate to Telehealth. In a nutshell, HSA regulation states that employers can't provide “significant care" before a qualified HDHP kicks in. However, the word “significant” was never specifically defined. So, the question became: is a $0 visit fee Telehealth service considered “significant” care?
Regulators had not specifically answered this question until the CARES Act came along. This Act clarified that $0 visit Telehealth can be provided alongside an HDHP without invalidating the tax-free status of an HSA. This rule is in effect for plans that begin on or before 12/31/21, so take advantage while you can and we’ll see if this is extended post-COVID19.
Here is a list of common Telehealth payers…
- Carriers: after changing policies to cover Telehealth more broadly during the beginning of the pandemic in 2020, some insurers started scaling it back as soon as they were allowed. Click here to learn more.
- Employers: purchasing direct from Telehealth companies or through standalone companies.
- Patients: some choose to purchase their own Telehealth plan direct from telehealth companies, through standalone companies, or one-off consults through doctor scheduling services.
- Medicare-Medicaid: since the start of the pandemic, there have been 31 major federal policy changes, including allowing Medicare patients to have telehealth appointments at home, reimbursing for more types of visits, and a temporary loosening of HIPAA restrictions to allow visits to be conducted over more types of platforms. There are big questions about how much of this will go back to normal – or if some of the changes will stay in place.
- Universities/unions/associations: some schools purchase telehealth plans direct from telehealth companies, or through standalone companies. Unions/Associations also purchase plans as part of their membership benefits.
It now appears that the regulation for payment of telehealth visits is going to be a huge discussion point in 2021. Some representatives & physician groups believe they need to pass a law guaranteeing providers pay parity for virtual visits. They argue that if a doctor has a visit via Telehealth, they should be paid the same amount as if they had seen the patient in person. Click here and go to page 11 to learn more.
PREDICTION #2
First, I hope you can now see how my first prediction might be possible! Before I share prediction #2, a little story: we’ve been including Telehealth in our plans since 2009. At that point, we thought we were late to the party. Eleven years later, many health plans don’t include basic Telehealth – and most charge a visit fee for it.
You might think these new telehealth options will start getting baked into the plans – we thought that 11 years ago.
PREDICTION #2 The best care and innovations will be provided as standalone services outside of a health plan.
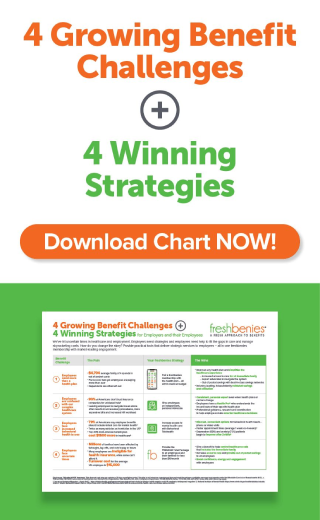
The good news for employee benefits consultants: this gives you something else to SELL – and allows you to be a more comprehensive consultant and bring even more value to your clients.
I encourage you to think and learn about all the ways you can use Telehealth to help your clients over time.
Now it’s your turn! How do you see these trends impacting consumerism healthcare behaviors? What predictions would you make? Comment below or email me at heidi@freshbenies.com.