4 Benefit Considerations to Help Employers Through Tough Changes
No question, the impact of COVID-19 is far-reaching. From the three million plus cases, with nearly one million cases in the U.S., to the loss of 200,000 lives worldwide - it’s like nothing this generation has experienced.
Beyond the health statistics, since mid-March over 26 million jobless claims have been made in the United States. Millions of additional employees have been furloughed. Employers of all sizes face the moral and financial dilemma of evaluating employee headcounts. As a benefits consultant, how can you help?
Today, I’m sharing four considerations to discuss with your clients who face tough team and benefit decisions.
Of your employer clients, you likely have…
- some who are considering furloughs (or other types of approved leaves of absences to reduce immediate payroll) hoping the downturn lasts for a period of weeks instead of months
- others who are opting to implement systemic reductions in the workforce and let employees go.
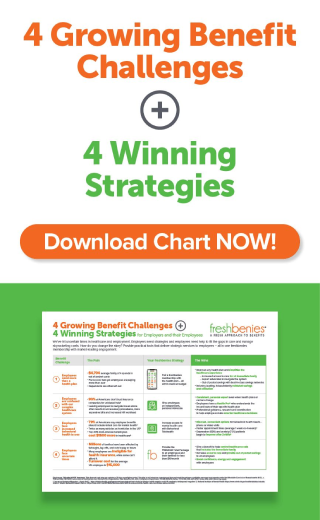
Different employment actions produce different employee benefit consequences. While no general rules apply to every situation, I’ve compiled a list (including some insights from SHRM - Society for Human Resources Management) of key considerations employers should evaluate when it comes to benefit programs and reducing payroll costs.
1. Determine if coverage continues during leaves or furloughs, or automatically ends upon termination of employment.
Plan terms typically dictate whether active coverage can continue during short-term leaves of absence - whether paid or unpaid - and many plans have minimum hour requirements to maintain active coverage. Employers that expand coverage for ineligible employees outside the terms of the plan or policy without consent from the insurer or stop-loss carrier face significant financial exposure.
2. Understand that COBRA continuation coverage (or state continuation coverage, if any) generally must be offered for all group health plans.
This applies when there is a loss of coverage due to termination or reduction in hours, as well as a furlough. An increase in the employee's share of the premium because of his or her reduction in hours (including to zero, as in a furlough) is a loss of coverage for this purpose.
3. Consider the Affordable Care Act (ACA) employer penalty.
Terminating the group health plan coverage for an employee when a leave or furlough begins may cause an ACA penalty for failing to offer coverage to 95% of full-time employees. COBRA coverage must remain affordable to avoid an ACA penalty, which may require a continued or increased employer subsidy.
4. Investigate non-insurance solutions that can provide quick, affordable options.
There are benefits that can be quickly enacted to help recently furloughed or laid-off employees - without limiting insurance rules. Such services can provide quick access to care, be launched at any time, used as often as needed, have no health restrictions, and be canceled at any time.
As you help employer clients navigate strategic business decisions alongside the desire to take care of employees and their families, the freshbenies team stands ready to help.
The non-insurance services in a freshbenies membership provide a wide range of help - from virtual doctor and behavioral health visits to expert Advocates to find resources available for financial assistance, insurance assistance, local COVID-19 testing and more.
One freshbenies membership helps employees and their families control and easily access healthcare - whether they have insurance or not. Plus, it’s inexpensive (employer-paid plans are $10 or lower, per employee family per month) and can be provided to employees of ANY status...
- full-time
- part-time
- furloughed
- departing
If we can help, our team’s here to serve you and your clients with fast set-up and best-in-class service.
Now it’s your turn. What client needs are you seeing in this new climate? Comment below or email me at neil@freshbenies.com - and reach out if I can help you strategize on some specific groups.