HLTH CONFERENCE 2019: TOP 10 TAKEAWAYS
We just returned from the second annual HLTH Conference at MGM Grand in Las Vegas and it did not disappoint again this year (click here to read my 2018 takeaways). HLTH (pronounced “health”) is a one-of-a-kind ecosystem event for the health industry. The mission is to bring together 6,000+ senior leaders from across payers, providers, employers, investors, fast-growing startups, pharma, policymakers and innovation centers - to solve the most pressing problems facing healthcare today and actualize the most promising opportunities to improve health.
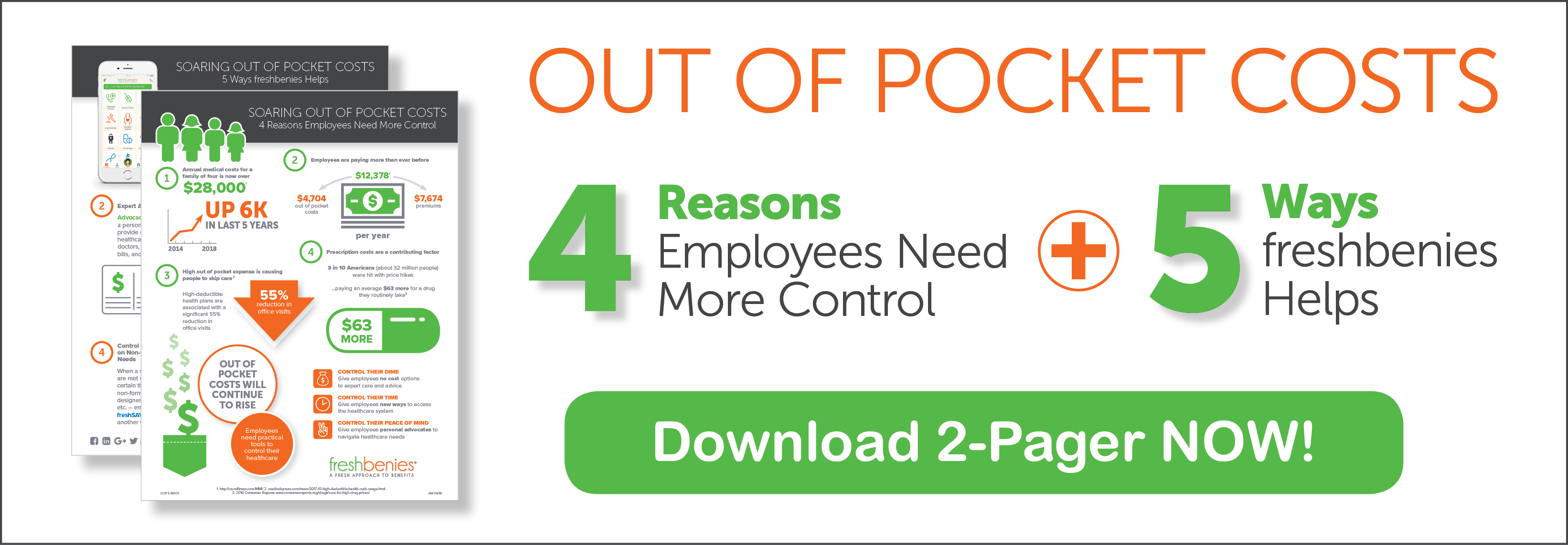
Since we spend most of our conference time at employee benefits events (click here for a list of our favorites), our goal was to see what was happening in healthcare as a whole – and to find new ideas to help our freshbenies members control their healthcare.
Below are our top 10 takeaways from the conference…
1. Patient experience – care at home
According to HLTH, “Studies show recuperating from a health event at home leads to significantly faster recovery times and reduced readmissions, not to mention costs 52% less than hospital stays. Health leaders are taking notice of the stats and creating sophisticated care models centered around treating patients in the comfort of their own home.”
As more care is delivered outside the four walls of a hospital or clinic, it’s critical to build improved patient experiences that lead to better outcomes. There were leaders from companies like Contessa, Alive Cor and BioIntellisense that offer medical grade monitoring and care for home use versus in a hospital room.
“Most of today’s healthcare interactions are not for the consumer. They’re for the healthcare system. We need to rethink and redesign how we engage consumers,” Dr. Freddy Abnousi, Head of Healthcare Research, Facebook.
“The exam room of the future will be your home - using technology to identify situations before they go very bad,” Ann Mond Johnson, CEO at American Telemedicine Association.
2. Improving the delivery of care
According to HLTH, “True patient-centered healthcare is the holy grail for most institutions. How do we design our operations around keeping our patients’ needs priority number one? What challenges hinder our efforts?”
Marcus Osborne, VP Health & Wellness Transformation, Walmart noted “40% of Americans who received care last year said it was not good service.” He shared a fully integrated care experience in Dallas, Georgia that Walmart is piloting. Medical, dental, vision, behavioral health – all under one roof and with very affordable pricing.
Technology must amplify the human experience and take the friction away. “We’re too far behind {in healthcare} – think of walking through the airport and using your phone or watch to get timeline updates, change of gate information, or to show your boarding pass,” notes Sven Gierlinger, a former luxury hotel executive turned Chief Experience Officer, Northwell Health. Why can’t we do that with our healthcare?
Dr. Adrienne Boissy, Chief Experience Officer at Cleveland Clinic noted, “As our patient, we should know (and capture) your preferences, values, concerns. This leads to building predictive models for patient care and engagement that matches patient preferences.”
President of Best Buy Health, Asheesh Saksena, discussed care that doesn’t hinge on first actions being taken by the patient. With their Lively Home approach, sensors are passively gathering info from a senior – when something changes, a personal call to the individual is made. For example, a sensor showed a senior was opening his fridge less often. A care call to the senior revealed that food no longer tasted good to him. He hadn’t reached out to a doctor, but through an inbound call and conversation, care steps were put in place.
Larry Merlo, President and Chief Executive Officer of CVS Health says we need to consider all the activities before and after a patient is in a physician’s office. What if medical and pharmacy data were merged to deliver a differentiated experience? For example: when a prescription is picked up, the pharmacist could remind a diabetic patient that they’re due for an A1C check. Or, if a patient received their post-surgical discharge checklists prior to a procedure, needed items and physical therapy coordination could be planned in advance so the patient goes home with those needs in place. These actions not only improve the patient experience, they also lower costly hospital readmissions.
3. Telehealth/Telemedicine
According to HLTH, “Speculation around the adoption rates of telehealth has led to many debates on whether consumers are really ready to embrace this new method of care. With greater access to telehealth, new data to support its effectiveness, and an increased focus on behavioral health benefits, the door is wide open for widespread adoption…Telehealth is quickly evolving beyond the state of urgent care and into the mission-oriented realm of delivering a greater level of dignity to some of our most vulnerable Americans.”
Telehealth was mentioned in many sessions and there were providers for all types of medical specialties throughout the exhibit hall. Click here for an article we wrote earlier this year about how we can leverage this innovation for more than just acute care needs.
“Telehealth usage doesn’t usually grow due to a DEMAND curve, but rather due to a CONVENIENCE curve,” Fay Rotenberg Bush, President, Firefly Health.
Dr. Peter Fleischut, SVP and Chief Transformation Officer, New York - Presbyterian Hospital noted, “The time will come when we don’t talk about ‘in-person health’ and ‘telehealth’ - when we just call it ‘health.’ We view the experience now as a consumer health journey. People should be able to get care where and when they need it.”
CEO of Crossover Health, Dr Scott Shreeve, painted a compelling vision of how we, as an industry, need to build a system that works smoothly from the physical delivery of care to the digital delivery of care and back again. He simply, but astutely noted, “It’s not complicated, it’s just really hard.”
4. Behavioral Health
According to HLTH, “The relationship between emotional and physical well-being has been established. What’s not established is fully incorporating mental health into the workstream of managing and monitoring whole health.”
Let’s not forget the need for this medical specialty. 36% of Gen Z and Millennials together say they’ve reached out for behavioral health help in the last 6 months. And 80% of counties don’t have even one psychiatrist. This creates obvious in-network, accessibility, and value issues.
Mark Coffin, Houston Office Managing Partner and Chair of Business Services Group for Seyfarth Shaw, LLP says meeting behavioral health needs means interorganizational support, tools, coaching, and a provider doing more online access in multiple channels to get the right kind of program with preferred engagement methods of employees (text, email, call, etc.). He sees these types of robust behavioral health programs as a way to tell people their company cares – which also helps to retain and recruit.
Citi’s SVP of Global Benefits, Niko Triantafillou, says they had very low utilization of their EAP program, but now have revamped to include 7-8 different ways to access behavioral health - from onsite counselors in their largest offices to telemedicine behavioral health by phone or video. They also led an effort to have executives talk candidly about mental health issues to destigmatize using the services.
“Virtual behavioral health is as good or better than in-person, in many ways,” noted Ann Mond Johnson, CEO, American Telemedicine Association.
5. Chronic condition management
According to HLTH, “6 out of 10 adults in the US have a chronic disease. We are afflicted from head to toe and desperate for innovations that ease our conditions. Ingenuity, technology and tenacity can provide preventative care and condition management to our disease-plagued population.”
In short, there were multiple ideas about how to do a better job helping people with diabetes, heart disease, hypertension, Alzheimer’s, etc. Some solutions used AI and Machine Learning to help identify patients at risk for developing chronic conditions. For those who were already diagnosed, AI and Machine Learning are being used to predict flare ups. There are also new pharmaceutical solutions, and customized, condition-specific telehealth services to make it easier for people with chronic conditions to stay healthier.
6. Tech, tech and more tech
According to HLTH, “We are living in a tech-centered world! With an ongoing mission to add intelligence and convenience to our daily lives, the health industry has embraced the latest tech…”
Some examples:
- Pharmaceutical companies are bringing in Chief Digital Officers to launch patient-centric technology that improves access and adherence to medications
- Artificial Intelligence for everything from early detection of disease, to streamlining back-end administrative processes and taking over time-consuming workflows, to providing insights that improve outcomes and lower costs
- Genomics bring new data about DNA-inspired behavior changes and genetic clues into more common conditions
- 3D printing for devices, tissues and even organs (someday)
- Advancements in robotics for less invasive surgery
- Virtual Reality to alleviate pain
- 5G superpower will allow faster imaging, expanded telemedicine, and reliable real-time remote monitoring
- Voice technology and smart speakers that engage consumers in all aspects of their healthcare
- Blockchain for something, but we can’t really figure it out!
Dr. Freddy Abnousi, Head of Healthcare Research, Facebook left us with a great reminder: “We need to design for people. Design with the person in mind. We don’t want tech for tech’s sake. If something doesn’t improve the outcomes, I don’t want it. If it does, then we should move in that direction.”
Philip Hess, CEO and President of Bose said, “If we put the best of consumer electronics with the best of healthcare, great things could happen.”
7. Government involvement
Obviously, healthcare is a complex industry with its share of government intervention, but we still need non-partisan solutions to increase access to affordable health care.
Because of this, Paul Markovich, President and CEO, Blue Shield of California observed, “We need to get away from a bumper sticker discussion on healthcare.”
Mark Cuban had some words for DC when he pointed out, “People are tired of solutions that are supported only by the one political party.” Yes, Mark Cuban. See #10 for more on his plan of action!
We heard from Tomas Philipson, Acting Chairman of the Council of Economic Advisers at The White House who said, “Medicare For All would be a tax-financed government monopoly.”
And finally, Seema Verma, Administrator of the Centers for Medicare and Medicaid Services (CMS) shared some scary statistics: “There’s the broader question of the financial sustainability of our programs which has swelled considerably. My budget at CMS is about $1.3 trillion – almost a third of the federal budget and more than the department of defense –and it’s expected to grow even more. We’re adding 10K new beneficiaries every day in Medicare – and the Medicare trust fund is projected to be insolvent by 2026. Medicaid has become the first or second largest budget item for most states crowding out other priorities such as roads and education. And Medicaid is the largest payer of long-term care – so imagine how the aging baby boomer population will exacerbate these problems. And between 2014 and 2050, Medicaid spending on those needing long-term care is expected to balloon from $68B to $401B. We can’t afford to meet our current obligations as it is – and you don’t have to be a mathematician to realize that Medicare For All as a public option would only accelerate our financial challenges. What these examples show is that the government has already stepped well beyond its proper role and is contributing to an unsustainable system.”
8. Social determinants
According to HLTH, “Community meets compassion meets commission. All across America, local, state and federal entities are aligning geographically and sociologically to organize health services and resources around the Social Determinants of Health.”
As one example, Dan Trigub, Head of Uber Health, shared how his company is working to remove transportation as a barrier to care. Approximately 15.5 million Americans 65 and older live in communities where public transportation service is poor or non-existent. Cerner and Uber are collaborating to help get patients to and from their doctor appointments – addressing a major social determinant of health that hinders the cost-effective management of chronic conditions.
Andrew Parker, Founder & CEO of Papa, noted that 80% of health problems driven by social factors – like lack of good food, housing, transportation, etc. The theory is that if we can improve those social factors, health problems will decrease.
9. New entrants & partnerships
According to HLTH, “Boundaries defining the health industry are receding as retail, banking and finance, transportation, and other industries are advancing into the health space. What trends can we expect as a result of this blurring of industries and who is taking the lead in reshaping health?”
- Uber is partnering with health plans and providers to remove transportation as a barrier to care
- Amazon, Berkshire Hathaway and JPMorgan Chase announced a collaboration to do something about healthcare for their employees
- Best Buy partnered with Tytocare introducing technology like smart thermometers, personal EKG monitors, TytoCare's medical exam kit for online doctor visits, and other smart health devices
- Walmart announced their new Health Center concept
- Bose sees themselves as an audio wearable company playing for the long run
- Facebook is taking a run at healthcare
- Mastercard is working on FSA/HSA cards, biometrics and healthcare data security
- Microsoft announced a partnership with The Jackson Laboratory to create products that empower oncologists and researchers to recommend more personalized treatments to cancer patients
10. Bold ideas to fix the US healthcare system
As if numbers 1 through 9 weren’t chocked full of enough “bold ideas,” we heard from the following people who had newer ideas…
- Walmart is seeing great success with Centers of Excellence, a national pilot with Grand Rounds to help employees navigate the healthcare system more efficiently
- Crossover Health CEO Scott Shreeve shared his vision for bringing people, their doctors, data, and benefits together under one connected system
- Seema Verma, who manages a $1.3 trillion CMS budget which probably makes her one of the most powerful women on earth, is concerned about rising costs (see #7) and declared, “The solution isn’t rationing care – and it’s certainly not more government control or taxes. Rather, we must realign the payment paradigm in government programs to create incentives that deliver the outcomes we want – prevention of disease, higher quality of life, lower cost.”
- Mark Cuban has money, drive, time and curiosity, so he’s building a real proposal for a healthcare system of the future. And I really look forward to hearing more!
A few days after the HLTH conference, John Nelson, CEO at Warner Pacific Insurance Services, reflected about the conference, “I learned a lot, but not sure what.” I can agree with him. The entire industry continues to make great strides in new developments and there are plenty of non-healthcare companies who want to be a part of the fun. Most have learned to say “this will save money” whether it will or not (thank you, Health Validation Institute). Those making advancements seem to want the insurance market to fund everything and the American public doesn’t want to pay the bill for everything.
In the end, I think the biggest takeaway for me is that there are emerging tools to help Americans control their healthcare – and new lessons about how to better engage them to do so. Now, I just need to continue to find the best solutions for our clients to keep freshbenies “fresh.”