CONSUMERISM TOOLS: TELL YOUR CLIENTS TO EAT THEIR VEGETABLES
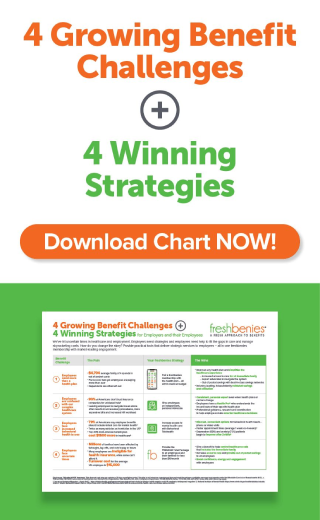
What’s the #1 reason an employer makes the decision to stop offering freshbenies? First, let me say this doesn’t happen often. But, when it does, we like to ask why they’ve made the decision to leave us. Almost always the answer is that their employees aren’t using the benefits, but they quickly follow up by taking the blame and saying that they didn’t do a good job of promoting the services.
They’re right, of course: if the employees don’t know what benefits they have or how to use them, utilization will be low. However, that doesn’t mean they should cancel the program; instead, they should remember why they decided to offer the benefits in the first place and redouble their efforts to educate their employees.
I’m going to stop short of blaming the employer, though. In my opinion, it’s the broker’s job to make sure the employees understand and take advantage of the benefits they have available to them. After all, the broker felt strongly enough that the services we offer—telehealth, doctors online, advocacy, and prescription savings—were a good solution that he recommended them to his client. Isn’t it his job to make sure those benefits are communicatedeffectively?
Imagine a parent saying, “I’ve stopped cooking vegetables because my kids won’t eat them.” That’s not a good answer. Kids need vegetables, and it’s the parent’s job to make sure they eat them. If that’s not happening, they need to try something different.
Consumer Tools Aren’t Optional
The consumer tools we offer are a lot like the vegetables that kids may not want but most definitely need. Think about it, nobody really wants a consumer-directed health plan. At its core, it’s a higher deductible plan with no up-front copayments. Prior to the deductible, people have to pay the contracted price for healthcare services and are asked to “shop around” and make better decisions, but right now there’s no good way to compare those options. Yes, people with this plan design can set aside tax-free dollars to pay for some of those services that were previously covered by copayments, but there are a couple problems:
1) Americans aren’t very good at saving money.
2) With today’s premiums, there’s not a lot of extra money to put into an HSA.
In short, we’ve tried to put a bow on these high deductible health plans and pitch them as a good thing, but employees don’t always see it that way. In their minds, they have a plan that “doesn’t cover anything.”
To make today’s plan designs a little more palatable to employees and to make sure they don’t go without needed care, we have to provide them and their family members with some alternatives:
- Telehealth services help to replace the missing copayments by letting people talk to a primary care doctor over the phone and get a prescription if medically necessary.
- Doctors Online services help people save specialist visits by getting their medical questions answered via email.
- Advocacy services help consumers find lower-cost providers and negotiate out-of-network claims, two behaviors consumerism attempts to encourage.
- Prescription Savings programs give employees an alternative to the discounts available through their health plan, help them understand that different pharmacies contract at different prices, and are a great starting point for consumers who want to shop for better deals.
We’ve said it for years: if we’re going to require consumers to take a more active role in their healthcare decisions, we have to give them the tools with which to make those decisions. Without price transparency and without additional options, it’s not really a consumer-directed approach; instead, it’s just a watered down health plan. These tools are absolutely necessary to promote consumerism in healthcare.
Communication is Key
If consumer tools like telehealth and prescription savings programs are an essential ingredient in a consumer directed approach, and if consumerism will almost certainly grow for the foreseeable future, then failing to offer these tools isn’t really an option. But we must recognize the fact that merely offering them isn’t enough; we have to make sure employees not only understand but are actually using them.
This is easier said than done. The truth is that most people don’t listen when they’re first told about their benefits, and those that are listening either won’t understand or will quickly forget what they’ve heard. That’s why it’s so important to tell them multiple times and in multiple ways. Talk about it in enrollment meetings. Show videos. Hang posters in the break room. Distribute flyers throughout the year. When someone calls in sick, ask if they’ve used their telehealth service. When an employee asks an HR manager for assistance with a bill, direct them to their advocacy service. Send information to the employees’ homes so their spouses will learn about the benefits too.
Is it easy? No. Is it necessary? Absolutely. Will the hard work pay off? Without a doubt! At freshbenies, we have tons of clients who are doing it right, and they and their employees are saving thousands of dollars a year. The bundle of services we provide isn’t an ancillary benefit for these groups, it’s an integral part of the health benefits. If your clients have low deductible plans with affordable up-front copayments, generous formularies, broad provider networks, and reasonable monthly premiums, they may not need these consumer tools. But if they’re like most groups nowadays, if they’re offering less comprehensive plans and asking their employees to share more of the cost, these sorts of solutions are no longer optional. It’s time for your clients to eat their vegetables.
Now it’s your turn. What effective communication strategies have you implemented with groups to raise employee awareness of benefits? How much responsibility do you think the broker holds for educating employees about new consumerism tools? Comment below or email me at eric@freshbenies.com.