COST-SHARING SUBSIDIES: 6 IMPORTANT QUESTIONS ANSWERED
In addition to the premium tax credits that people have heard a lot about, the Affordable Care Act also created “cost sharing reductions” (CSRs) to help low-income individuals pay their out-of-pocket expenses. Before President Obama left office, then-Speaker John Boehner and the Republican congress sued the president over these cost-sharing subsidies, saying that Congress had not authorized the payments his administration was making to insurers. Since then, the CSRs have been a political football, which means that almost every time we hear about them on the news, the information is mostly one-sided.
With so much bad or at least incomplete information out there, and considering that President Trump recently canceled the CSR payments to insurers, it seemed like a good time for a quick update. For brokers who sell individual products, you’re no doubt getting questions about the cost sharing subsidies from your clients.
I’m answering 6 hot topic questions every broker should know…
What are the cost-sharing reductions?
The cost-sharing reductions were created by the Affordable Care Act and first became available in 2014. The subsidies reduce people’s out-of-pocket exposure while increasing the actuarial value of their health plan. In English, that means the consumer pays less and the insurance company pays more for their healthcare expenses. There are three tiers of cost-sharing subsidies based on the family’s household income:
|
Income as a % of federal poverty level |
Reduction in out-of-pocket exposure |
Actuarial Value for silver-level plan |
|
100-150% |
Two-thirds |
94% |
|
150-200% |
20% |
87% |
|
200-250% |
20% |
73% |
Who qualifies for the cost-sharing subsidies?
To qualify for cost-sharing reductions, individuals and families must have incomes below 250% of the federal poverty level (FPL) and must purchase a plan in the silver-level of the state or federal marketplace.
|
Family Size |
100% of FPL |
150% of FPL |
200% of FPL |
250% of FPL |
|
1 |
$12,060 |
$18,090 |
$24,120 |
$30,150 |
|
2 |
$16,240 |
$24,360 |
$32,480 |
$40,600 |
|
3 |
$20,420 |
$30,630 |
$40,840 |
$51,050 |
|
4 |
$24,600 |
$36,900 |
$49,200 |
$61,500 |
|
5 |
$28,780 |
$43,170 |
$57,560 |
$71,950 |
|
6 |
$32,960 |
$49,440 |
$65,920 |
$82,400 |
Have cost-sharing reductions ended?
The short answer is: no. On October 12, President Trump signed an executive order promoting healthcare choice. In it, he called for the creation of association plans, longer terms for short-term health plans, and more creative uses of Health Reimbursement Arrangements. That same day, he announced an immediate halt to the cost-sharing reduction payments to insurance companies.
This announcement was followed by a number of news reports claiming that the subsidies were being discontinued and that low-income individuals would be harmed. That’s not actually the case. The subsidies did not go away, and millions of people will sign up for those plans over the next several weeks - the open enrollment period began November 1 and ends December 15. What the announcement means is that the government will no longer reimburse health carriers for these more comprehensive plans.
In anticipation of a decision like this from President Trump, many insurance companies across the nation made adjustments to their rate filings for their silver-level plans. According to the Kaiser Family Foundation, this rate increase ranged from +7 to +38%.
Aren’t cost-sharing subsidies just insurance company bailouts?
The short answer is: no. This is how cost sharing reductions work:
- People apply for coverage through the Marketplace.
- Depending on their income and household size, the plans they are shown for silver-level coverage provide enhanced levels of coverage (lower out-of-pocket maximums and higher actuarial values) without an increase in premium. For the same price as other silver-level plans, which is significantly reduced after the premium tax credits these individuals also qualify for, they can sign up for more comprehensive coverage.
- The federal government is responsible for the higher claims costs and higher utilization that results from these more comprehensive plans. Instead of paying higher premiums, the government essentially serves as the insurer for this portion of the claims cost. It’s almost like an HRA paid for by the government.
- The government actually fronts a portion of the expected claims cost to the insurer to compensate them for the cost-sharing reductions. After the fact, the insurer and government square up the claims costs and an additional payment may be necessary.
Again, these payments aren’t a bailout. The government requires carriers to reduce the out-of-pocket expenses for people who qualify. The carriers follow the rules and offer these more comprehensive plans, paying claims along the way. The government is then supposed to reimburse carriers for the extra claims cost. Due to the latest executive order, that’s not happening. It’s sort of like hiring contractors who actually perform a job for you and then stiffing them on the payment…
Interestingly, the fact that carriers anticipated this decision and charged higher premiums for 2018 means the federal government will likely have to spend more for the premium tax credits than they would have had to pay for cost-sharing subsidies. In 2018 alone, the net cost to the federal government of ending the CSR payments will be $2.3 billion according to the Kaiser Family Foundation. The government’s decision not to pay its bills is costing taxpayers billions of dollars.
One other thing: because the premium tax credits are calculated based on the price of the second-lowest-priced silver-level plan in the marketplace, and because those premiums are higher as a result of the decision to stop reimbursing carriers for the cost-sharing reductions, every single person who qualifies for a tax credit (even if they’re not receiving a CSR) receives more premium assistance in 2018. This means that the net cost of bronze-level coverage for these individuals actually decreases, and millions of people now qualify for free coverage through the marketplace. Perhaps that’s why marketplace enrollment is up this year compared with last year.
Is there any hope for CSR payments?
A Senate committee headed up by Lamar Alexander [R-TN] and Patty Murray [D-WA] has been working on a bipartisan bill that would guarantee the CSR payments for the next two years, but it’s not yet clear whether President Trump will sign it if it does end up passing. After the failure of the Republican “repeal and replace” bills this summer, there have been calls for a bipartisan solution to fix some of the problems with the Affordable Care Act.
What about those who don’t qualify for a CSR?
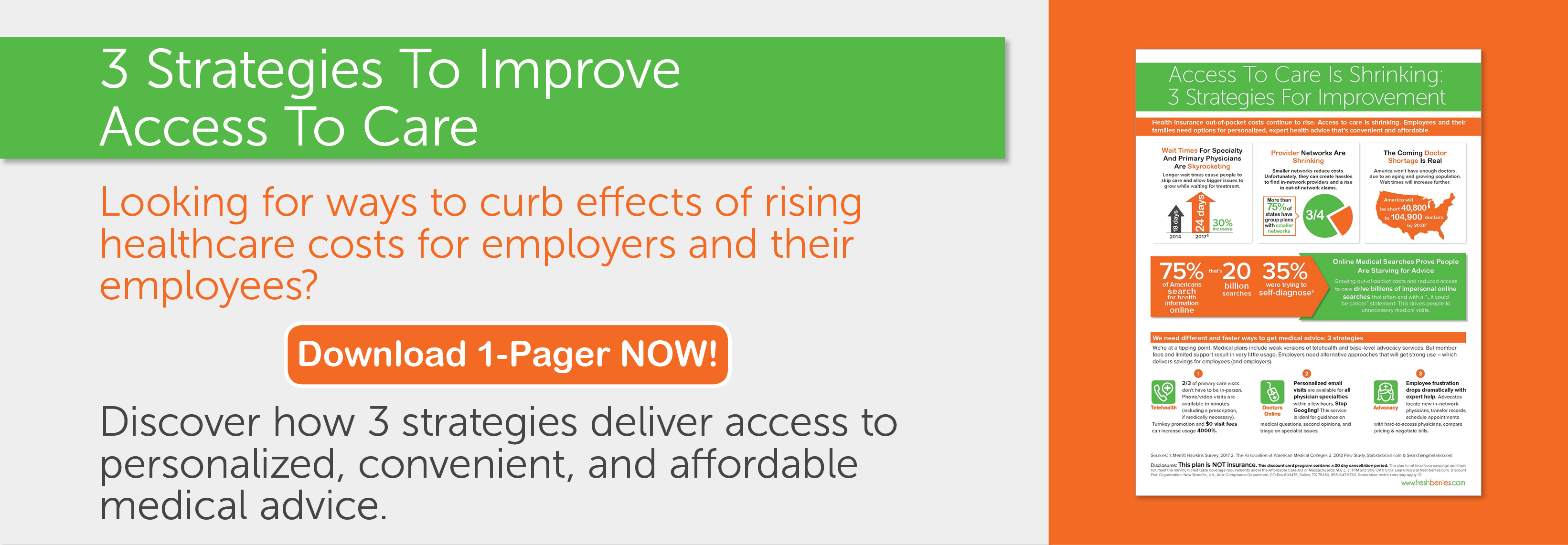
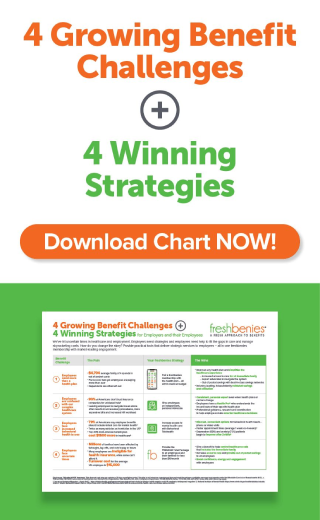
This is a very important question. While the cost-sharing reductions are great for those who qualify, the majority of people are ineligible either because their income is too high or because they have employer-based coverage available to them. Nearly everyone not receiving a cost-sharing subsidy, whether they have coverage in the individual or group market, has high out-of-pocket exposure nowadays and needs some resources outside the health plan to help reduce their out-of-pocket costs.
This is where tools like telehealth and doctors online, which give members access to a doctor by phone or email, patient advocacy, which can point members toward lower-cost providers and help negotiate bills for out-of-network services, and prescription savings programs, which help people save money on their medications, can be so valuable. As more and more benefits are pulled out of the health plans, brokers must supplement the health insurance they’re selling with first-dollar benefits their clients will actually use.
This is especially important in light of a January Bankrate survey, which found that nearly 6 in 10 Americans could not pay an unexpected expense of $500 or more. As Mark Bellman with UnitedHealthcare pointed out in a recent continuing education class, we have to ask ourselves if we really know our audience. Yes, the high-deductible, consumer-driven plans we’ve been recommending for years are great for a certain percentage of the population, but it appears that more than half of adults would really appreciate first-dollar benefits. Please keep that in mind as you’re advising your clients and designing benefits packages during this very busy time of year.
Now it’s your turn! How do you curb rising out-of-pocket exposure in your group plans? What types of conversations are you having with your clients on this topic? Comment below or email me at eric@freshbenies.com.