Is Free Telehealth Coming to an End? 5 Ways freshbenies Can Help
No doubt, 2020 has been a turbulent year. The continuing global pandemic has dramatically changed the way we live, work, socialize — and also the way we consume healthcare in the United States.
As the country learned to avoid public places and large gatherings, we were also counseled to avoid hospitals and other care locations unless absolutely necessary. Many carriers opted to expand telehealth benefits and some began paying for its use at the outset of the COVID-19 crisis — adding to the surge of telehealth awareness and use.
Today I’m sharing how the landscape of free Telehealth continues to shift and how freshbenies can help.
Will expanded coverage of Telehealth continue?
Effective October 1, several private health insurers will no longer fully pay for virtual visits under certain circumstances — effectively reinstituting costs for patients reliant on the virtual care that has been heralded as a lifeline during the pandemic.
UnitedHealthcare has ended their expanded virtual visit benefit through which it was covering the full cost of visits for individuals who were seeing in-network providers virtually for medical issues not related to COVID-19. Anthem has also stopped waiving the cost of copays, coinsurance, and deductibles for virtual visits not related to COVID-19.
For patients seeking out virtual care, cost-sharing for a virtual appointment can vary widely. According to Statnews.com, depending on the nature of the visit, a telehealth appointment can cost in the ballpark of $100 to $400.
Cost-sharing passes some portion of that down to the patient, their clinic or hospital. It’s still not clear how much patients affected by these recent changes can expect to pay for telehealth visits. Nor is it clear how those costs will compare to copays for an in-person visit.
Uncertainties persist
Meanwhile, some commercial insurers who’d planned to end their expanded telehealth coverage have extended their Sept. 30 expiration date until the end of the year, and others could still make a similar move in coming days.
Time will tell how many other carriers follow suit and reduce their telehealth benefits. For many of the carriers, “free” telehealth was simply a stop-gap measure necessitated by the pandemic. For freshbenies, it continues to be a core benefit.
As your groups are transitioning from a no visit fee telehealth plan, consider that employees likely just became used to having it – and changed their habits to engage with telehealth first.
freshbenies to the rescue
Here are 5 ways freshbenies can help…
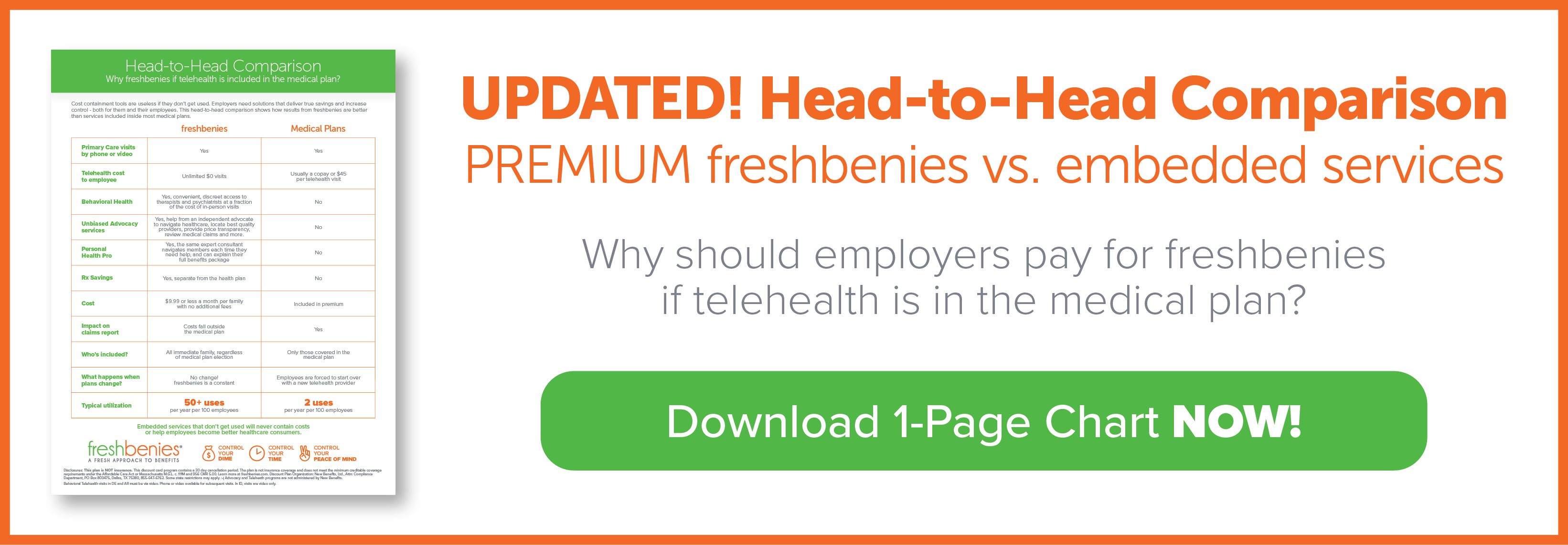
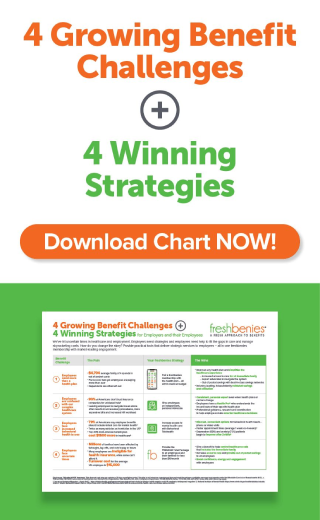
- Secure $0 telehealth visits without restrictions. freshbenies has always provided virtual primary care telehealth visits without a visit fee to our members (and their family members!).
- Add convenient, discreet behavioral telehealth access. Our PREMIUM package options offer a behavioral telehealth benefit that provides access to both therapists and psychiatrists at a fraction of the cost of a typical in-person visit.
- Leverage the telehealth momentum with additional consumerism tools. There are other virtual services bundled into one membership. Our premium Advocacy service provides resources that enable employees to make smarter, more cost-effective healthcare decisions.
- Give employees a benefit constant. Although medical plans can change and carriers easily switched, freshbenies can be a consistent resource to ease frustrations and help navigate benefit changes.
- Provide a benefit that contains cost. The freshbenies Member Engagement System works to educate employees on how, why, and when to use telehealth, advocacy and other freshbenies services. This drives high utilization and keeps unnecessary claims from hitting the health plan.
Now it’s your turn! How are you guiding groups through the shifting landscape of free telehealth? What additional consumerism tools are you recommending? Comment below or email me at neil@freshbenies.com.